Ulcerative Colitis: Understanding, Managing, and Thriving with It
If you or someone you love has been diagnosed with ulcerative colitis, you probably have a lot of questions. What causes it? How can you manage the symptoms? Is there a cure? Living with a chronic condition like this disease can be challenging, but with the right knowledge and lifestyle adjustments, it’s absolutely possible to lead a fulfilling life.
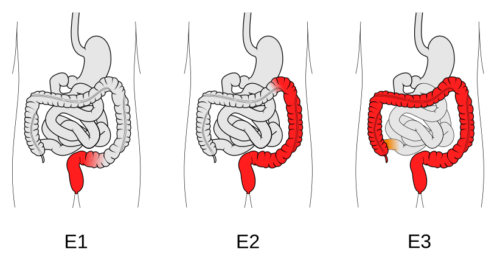
What is Ulcerative Colitis?
Ulcerative colitis (UC) is a type of inflammatory bowel disease (IBD) that causes long-term inflammation and ulcers in the colon and rectum. It’s not just an occasional stomach ache—it’s a serious condition that can significantly impact daily life. People with UC often experience symptoms like:
- Persistent diarrhea, sometimes with blood or mucus
- Abdominal pain and cramping
- Urgent and frequent trips to the bathroom
- Fatigue and weight loss
The severity of symptoms varies from person to person. Some may have mild flare-ups, while others experience more debilitating effects.
What Causes Ulcerative Colitis?
The exact cause of isn’t fully understood, but researchers believe it’s a combination of genetics, an overactive immune response, and environmental triggers. Instead of attacking harmful invaders, the immune system mistakenly targets the colon’s lining, leading to chronic inflammation.
Who’s at Risk?
- If you have a family history of ulcerative colitis, your risk is higher.
- It’s most commonly diagnosed in people between 15 and 30 years old.
- Certain environmental factors, such as stress, diet, and gut bacteria imbalances, may contribute to flare-ups.
How is Ulcerative Colitis Diagnosed?
If you’re experiencing ongoing digestive issues, don’t ignore them. A doctor may perform:
- 🔎 Colonoscopy or sigmoidoscopy – to check for inflammation and ulcers
- 🧪 Stool tests – to rule out infections
- 💉 Blood tests – to look for anemia and inflammation markers
- 🖥 Imaging tests (CT scan or MRI) – for a more detailed look at the digestive tract
Early diagnosis can make a huge difference in managing symptoms effectively.
Treatment Options for Ulcerative Colitis
While there’s no cure for it, various treatments can help manage the symptoms and prevent flare-ups. The right approach depends on the severity of your condition..
1. Medications
- 💊 Aminosalicylates (5-ASA drugs) – Help reduce inflammation in mild to moderate cases.
- 💊 Corticosteroids – Used for short-term relief during severe flare-ups.
- 💊 Immunomodulators – Suppress the immune response to prevent inflammation.
- 💊 Biologic therapies – Target proteins that cause inflammation (e.g., Infliximab, Adalimumab).
2. Lifestyle and Dietary Changes
Your diet and daily habits play a crucial role in managing it. Try these tips:
- ✔ Avoid trigger foods – Spicy foods, dairy, caffeine, alcohol, and high-fiber foods can sometimes worsen symptoms.
- ✔ Eat smaller, more frequent meals – Instead of three big meals, try eating five or six smaller ones.
- ✔ Stay hydrated – Dehydration can make symptoms worse, especially if you have diarrhea.
- ✔ Manage stress – Stress doesn’t cause UC, but it can trigger flare-ups. Try yoga, meditation, or deep breathing exercises.
3. Surgery (When Necessary)
In severe cases where medications don’t work, surgery may be required to remove the colon (proctocolectomy). Advances in surgical techniques, like ileal pouch-anal anastomosis (IPAA), allow many people to maintain normal bowel function even after colon removal.
Complications to Watch Out For
If ulcerative colitis isn’t well-managed, it can lead to serious complications such as:
- 🚨 Severe bleeding
- 🚨 Increased risk of colon cancer
- 🚨 Toxic megacolon (a dangerous expansion of the colon)
- 🚨 Osteoporosis (from long-term steroid use)
Regular checkups with a gastroenterologist can help catch and prevent complications early.
Living Well with Ulcerative Colitis
Being diagnosed with this disease doesn’t mean life has to stop. With the right treatment plan, lifestyle adjustments, and support system, you can live a healthy and active life.
If you’re dealing with it, know that you’re not alone. There are countless support groups, online communities, and medical advancements that can help you navigate this journey. Stay informed, listen to your body, and work with your healthcare provider to find the best path forward.
Explore more about health here. Click Me.